Sperm counts have been falling across the world for many years and the problem is showing no signs of slowing down 1 Levine H, Jørgensen N, Martino-Andrade A, Mendiola J, Weksler-Derri D, Mindlis I, Pinotti R, Swan SH. Temporal trends in sperm count: a systematic review and meta-regression analysis. Human Reproduction Update. 2017. 23(6): 646-659.. While scientists are unsure about the reasons behind the general worldwide decline in sperm count, many of the main individual causes of low sperm counts are well known. There are also many treatment options available for you to improve your chances of having a child.
What exactly is a low sperm count?
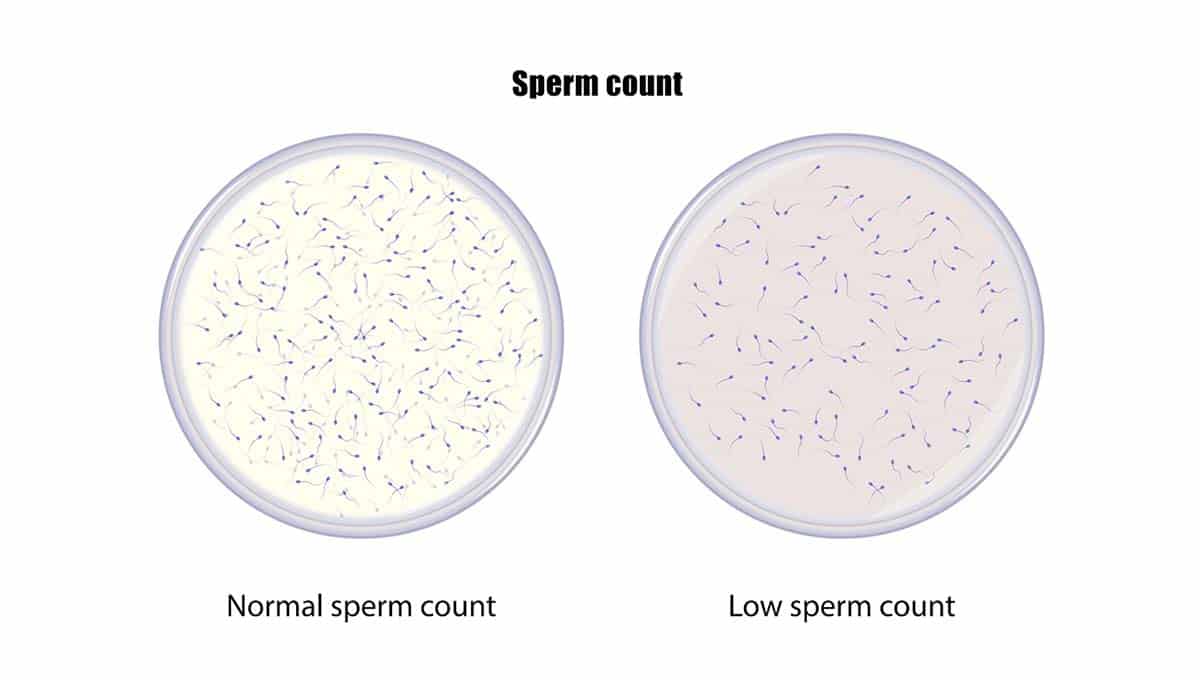
The term “sperm count” means the number of sperm cells in a sample of semen. A low sperm count means that you have fewer than 15 million sperm cells per millilitre of semen.
“Oligospermia” is the medical name for a low sperm count. If there are no sperm cells present at all in a semen sample, doctors call this “azoospermia”.
Is your sperm count actually low?
Before you panic, it is important to make sure that the test is accurate. Your sperm count could be normal but it might show as being low if there is a problem with the testing.
Low sperm counts can occur in error if:
www.amitamin.com/en/fertilsan-m New life deserves the best possible start!We provide the essential building blocks for this.
– A test was taken too soon after a previous ejaculation
– A test was taken too soon after an illness
– Some semen was spilled during collection
If you are in doubt about the accuracy of your results, it is a good idea to repeat the test after 1-2 weeks.
The most reliable way to monitor your sperm count is by testing several samples over a period of time. Sperm cells take 90 days to develop, therefore it is a good idea to test your sperm once every three months to detect any significant changes when you are trying to conceive.
What is the link between sperm count and fertility?
For a couple to conceive successfully, a sperm cell needs to fertilise an egg cell. This comes down to chance, therefore to maximise the likelihood of conceiving you should aim to have as many healthy swimmers as possible to reach and fertilise an egg.
But if a man has a low sperm count, fewer sperm cells are present and this reduces the chances of a successful conception. However this does not mean it is impossible.
This may just mean that it will take you longer to conceive with your partner. It might also take more attempts especially around your partner”s ovulation date as this can improve your chances of conceiving. It may also mean that you need some extra help in the form of fertility treatments.
In many cases, you can improve your sperm count with the help of treatments and lifestyle changes and this will boost your chances of conceiving. However this depends on the reason for your low sperm count, and you might need to discuss which options are best for you with your fertility doctor.

Symptoms of low sperm count
Many men only find out that they have a low sperm count after they have been trying to conceive without success for some time. In general, if you have been having regular unprotected intercourse for one year and have not conceived, it would be a good idea to see your GP or fertility doctor to check that you and your partner are healthy.
There are a number of other symptoms which can occur in men with a low sperm count. These include pain or a swelling in the groin, a low sex drive, erectile dysfunction, or reduced hair on the body or face. However the symptoms depend on the reason for your low sperm count, so you are unlikely to have all these symptoms together.
Causes of low sperm count
There are many causes of low sperm count. To understand these better, it is helpful to group them into three main categories: medical, environmental and lifestyle factors.
Medical causes of low sperm count
Varicocele
This is the most common cause of fertility problems in men. A varicocele occurs when the blood vessels inside the scrotum become dilated. It is helpful to think of them as the equivalent of varicose veins in the legs.
A varicocele usually occurs because the valves in the small blood vessels do not function normally. This can cause blood to pool and dilate within the blood vessels. This problem normally arises in teenagers and young men.
The good news is that varicoceles are treatable. They are also quite common, and many men have varicoceles without experiencing any problems with their fertility. In these cases, there is no need for treatment.
But in some men, varicoceles can cause infertility. Scientists are unsure why exactly this happens, but they think that the temperature is a key factor.
Many scientists believe that the pooled blood in the dilated veins increases the temperature inside the scrotum. The rise in temperature may be slight, but it can still be enough to cause problems as this part of the body is extremely sensitive to temperature. This change can have a harmful effect on the number and quality of sperm cells produced, which can result in fertility problems.
In men with fertility problems due to varicoceles, the usual treatment is surgery. This blocks the blood flow through the dilated veins and the blood is diverted through other vessels. This can be done as a minor outpatient procedure.

Problems with ejaculation
Many health conditions such as diabetes and spinal injuries can cause problems with ejaculation. Specifically, men may experience retrograde ejaculation or erectile dysfunction.
Retrograde ejaculation happens when the semen does not exit the tip of the penis through the urethra during an orgasm. Instead the sperm cells enter the bladder, and this problem can occur after surgery to the prostate or bladder. In erectile dysfunction, men can have problems developing and maintaining an erection during intercourse.
Ejaculation problems can result in infertility because the sperm cells are unable to reach their destination to fertilise an egg. Treatments are available in the form of medications. Counselling may also help in cases of premature ejaculation. If these options do not work, fertility treatments are still an option as the sperm cells are healthy.
Medicines
A number of medicines have the unwanted side effect of reducing fertility. One of the common culprits is alpha blockers. This is a class of drugs which is used to treat symptoms associated with an enlarged prostate.
Certain antifungal drugs and antibiotics can affect fertility too, as well as chemotherapy medicines. Anabolic steroids are widely used for boosting muscle mass, but they can also impair sperm development if they are used over a long period of time. This is a major cause of preventable infertility.
It is important to discuss the side effects of any medications with your GP and discuss alternative options if there is a significant risk of damage to your fertility.
Infections
Infections can affect the health and development of sperm cells. Infections can also damage the reproductive system by causing blockages and scar tissue. These infections include inflammatory diseases such as epididymitis, as well as some sexually transmitted infections such as gonorrhoea.
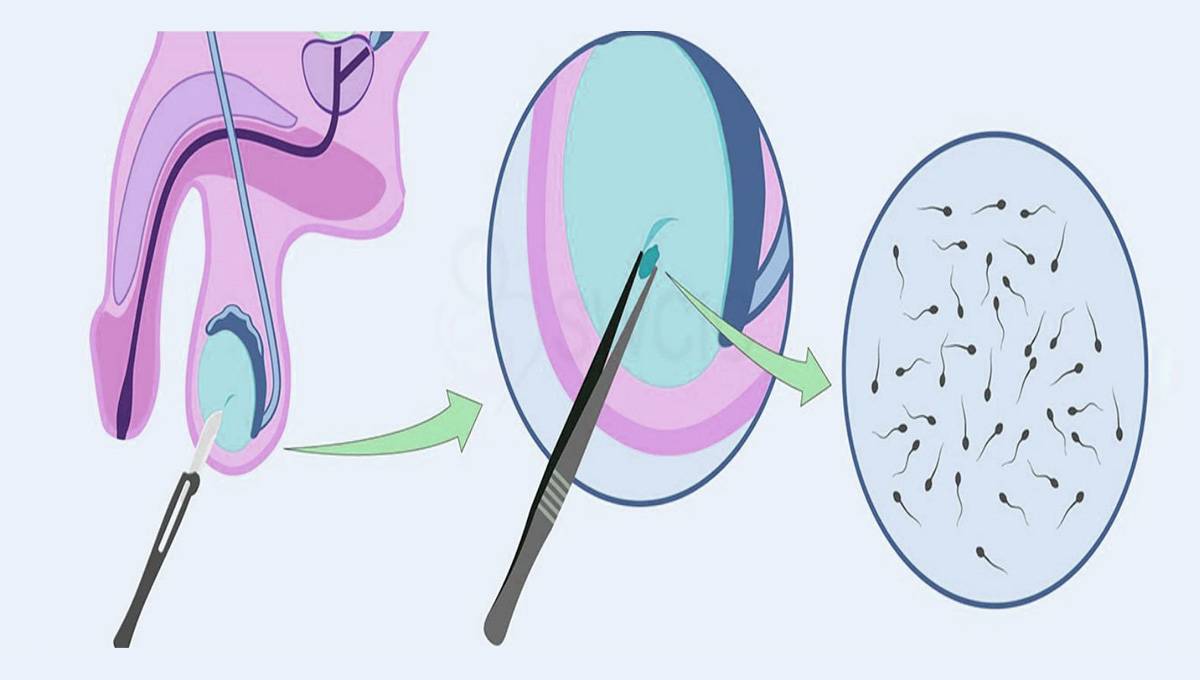
In acute infections, medications are the key treatment and it is important that these are started as soon as possible to prevent long-term damage. In cases where chronic infections have caused untreatable problems in the reproductive system, there is still hope in the form of a technique called “surgical sperm retrieval”. This enables healthy sperm cells to be gathered and used in fertility treatments such as IVF or IUI.
Undescended testicles
This is a common condition where one or both of the testicles have not moved down into the scrotum. The medical name for this is “cryptorchidism”, and in normal circumstances the testicles should descend before birth.
The treatment for undescended testicles can involve hormone treatment or surgery. But even after treatment, men who have had cryptorchidism in the past are more likely to be infertile.
The risk of infertility is higher if the problem affected both their testicles 2 Fawzy F, Hussein A, Eid MM, El Kashash AM, Salem HK. Cryptorchidism and Fertility. Clinical Medicine Insights: Reproductive Health. 2015. 9:39-43.. Men also experience worse fertility problems if their cryptorchidism was not treated quickly enough. This is because the testicles were exposed to higher temperatures until they reached the scrotum, which is cooler as it lies on the outside of the body. The extra time spent exposed to higher temperatures has a negative impact on sperm cell development.
Tumours
Tumours can either be malignant or benign, but in both cases they can affect male fertility. The exact effect depends on the characteristics of the tumour.
Tumours may affect fertility by directly compressing structures responsible for the passage of sperm cells. Their effect can also be indirect as they can alter the levels of hormones in the body which are responsible for sperm cell development.
Additionally male fertility can be affected by cancer treatments including surgery, chemotherapy and radiotherapy. The effect depends on the dose and the specific treatment used. Sperm freezing is a useful way to preserve your fertility in these cases.
Hormone problems
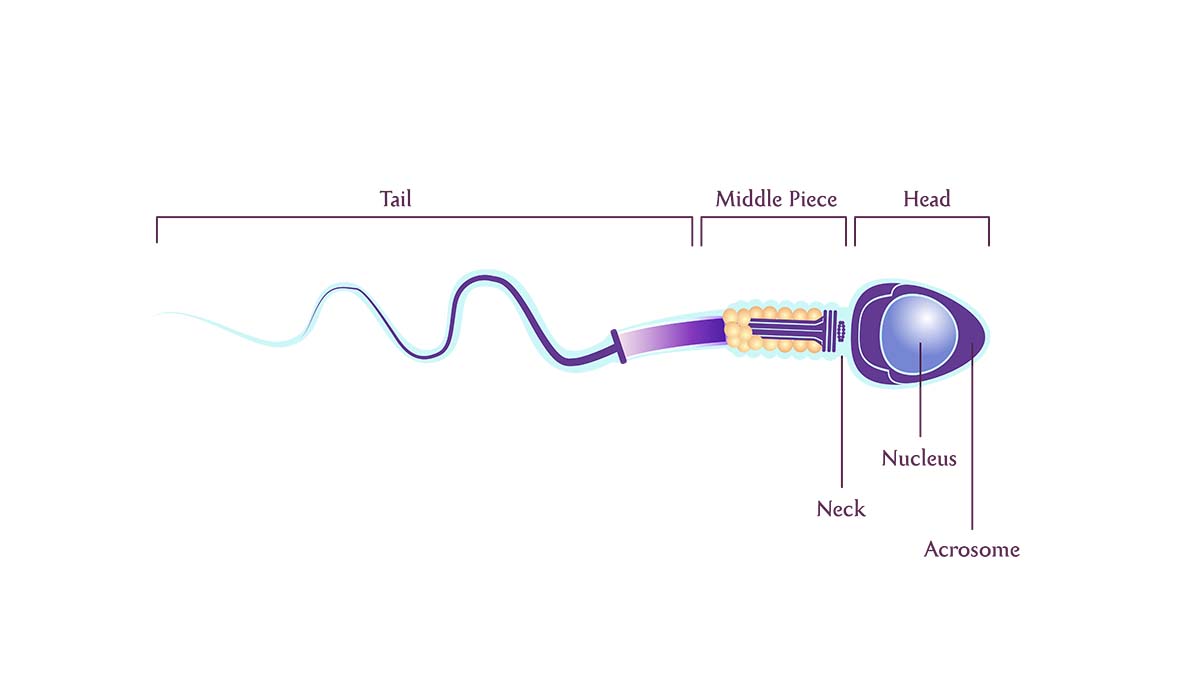
The sperm development process is controlled by hormones. These are chemical messengers which coordinate the actions of different parts of the body, and they include luteinising hormone (LH), follicle stimulating hormone (FSH) and testosterone.
The brain releases hormones from the pituitary gland and the hypothalamus. Together with testosterone released from the testicles, this creates a system which initiates and controls the healthy development of sperm cells.
If there is a change in any of the hormone levels, this will in turn affect the other hormones which will impact the sperm development process. The adrenal and thyroid glands also produce different hormones which can affect fertility. The treatment depends on the severity and type of hormone disorder.
Genetic conditions
These conditions are hereditary and they affect the genetic material inside the cells of the body. This means that these conditions can involve a range of symptoms alongside fertility problems.
Examples of genetic conditions which cause reduced fertility in men include Kartagener”s syndrome and Klinefelter”s syndrome. Although the condition itself may not be treatable, men may still be able to have a child with the help of medications and fertility treatments.
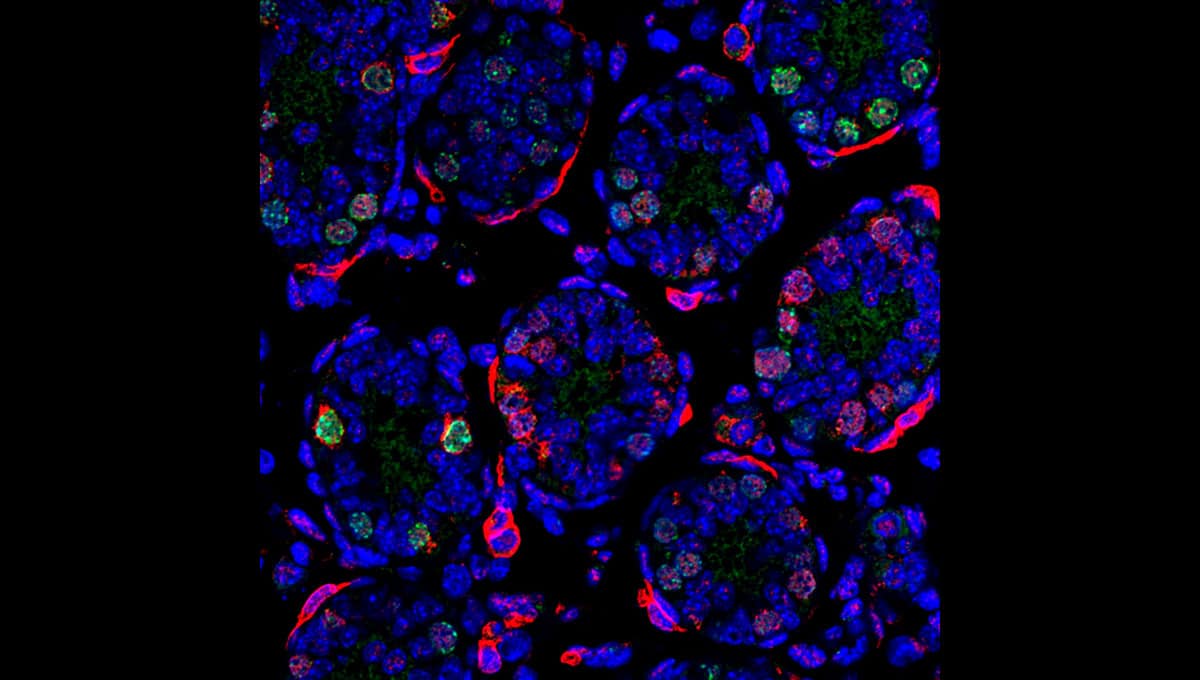
Transport problems
Sperm cells are transported through a network of vessels called tubules. If there is a blockage in the tubules, the sperm cells will not be able to exit the urethra and there may not be enough sperm cells in the ejaculate for fertilisation to occur.
Among patients with cystic fibrosis, the majority of men are infertile. The vas deferens is a tube which carries sperm cells from the testicles to the penis, and in men with cystic fibrosis the tube is missing or blocked. The tubules can also be blocked for other reasons including a traumatic injury or infection.
The good news is that the sperm cells themselves are healthy. This means that the sperm can be collected through a process called surgical sperm retrieval and they can then be used in fertility treatments.
Immune system disorders
Problems can arise when the immune system overreacts to certain molecules in the body. An example of this is coeliac disease.
Coeliac disease is caused by the body”s immune reaction against gluten. As well as gastrointestinal symptoms, coeliac disease can have a negative effect on male fertility. Fortunately fertility issues and other symptoms can improve if you follow a gluten-free diet 3 Freeman HJ. Reproductive changes associated with celiac disease. World Journal of Gastroenterology. 2010. 16(46): 5810-5814..
Antisperm antibodies are another immune problem which affects sperm cells directly. This can occur after an injury or vasectomy which results in blood and sperm coming into contact with each other, as usually they are separated. This results in the body mistakenly targeting sperm cells with antibodies which attempt to destroy the sperm. Men with this disorder can still have a child with the help of fertility treatments such as ICSI.
Previous surgeries
The most obvious surgery which affects male fertility is a vasectomy. Other examples include inguinal hernia repairs, prostate surgeries, and scrotal or testicular surgeries.
To repair the damage done to the reproductive system, you may need to undergo another surgical procedure. Alternatively, if the sperm cells are healthy they can be collected surgically and used in fertility treatments.
Mental health
Mental health requires just as much attention as physical health, as they both are interconnected. The data supports this as studies have found that depression and anxiety can reduce sperm count 4 Wdowiak A, Bień A, Iwanowicz-Palus G, Makara-Studzińska M, Bojar I. Impact of emotional disorders on semen quality in men treated for infertility. Neuro Endocrinology Letters. 2017. 38(1): 50-58..
Stress plays a huge part in controlling the body”s hormone levels. Cortisol is the body”s stress hormone, and high amounts of this can reduce levels of testosterone which impairs the sperm development process 5 Ilacqua A, Izzo G, Emerenziani GP, Baldari C, Aversa A. Lifestyle and fertility: the influence of stress and quality of life on male fertility. Reproductive Biology and Endocrinology. 2018. 16:115..
Therefore it is important to control your stress levels as much as possible by finding ways to relax. This might include making time for hobbies and reaching out for support from loved ones.
Exercise is an excellent way to relax. Moderately intense exercise 6 Maleki BH, Tartibian B, Chehrazi M. The effects of three different exercise modalities on markers of male reproduction in healthy subjects: a randomized controlled trial. Reproduction. 2017. 153(2): 157-174., yoga, and meditation techniques such as mindfulness (MBSR) have been proven effective at reducing cortisol levels.
But make sure that you do not use alcohol to help you relax, as there is a strong link between alcohol and reduced fertility in both men and women 7 Gude D. Alcohol and fertility. Journal of Human Reproductive Sciences. 2012. 5(2): 226-228..
If you need help, please discuss this with your GP. They will be able to help you access various sources of mental health support such as counselling.

Environmental causes
Your environment can have a significant negative impact on your health and fertility. But fortunately your exposure to these factors is within your control. Here are the environmental factors you need to look out for:
Radiation
A common form of radiation is X-rays, and they can affect fertility by damaging the health of existing sperm cells in addition to the development of new sperm cells.
The general rule is the bigger the dose, the more damage is done. The occasional X-ray is nothing to worry about as after low to normal doses of radiation, sperm counts can still recover. But after very high doses of radiation, the fertility damage can be permanent.
Toxins
Industrial chemicals can have a serious impact on fertility after long-term exposure. Occupational exposure to chemicals including herbicides, pesticides, benzenes and toluene can reduce your sperm count. Lead, cadmium and other heavy metals can also harm fertility.
High temperatures
Sperm cells are extremely sensitive to temperature. This is why Mother Nature ensured that the testicles are located outside the body, as this allows them to have a lower temperature than the rest of the body.
The major places to avoid are saunas and hot tubs, as they can make your testicular temperature soar. Your laptop can also get extremely hot, so make sure you are not resting it on your lap for long lengths of time. Also make sure your underwear and clothes are not too tight around your groin.
Lifestyle causes
Alcohol
Excessive alcohol consumption in the form of heavy binge drinking can lower testosterone levels and therefore reduce fertility in men. It can also cause erectile dysfunction.
To improve your sperm count, drink in moderation and try to reduce how much you drink on a daily basis. Make sure you avoid binge drinking and contact your GP for more support.
Smoking
Tobacco smoking can significantly lower your sperm count, as well as reducing the likelihood of success in fertility treatments 8 Kovac JR, Khanna A, Lipshultz LI. The Effects of Cigarette Smoking on Male Fertility. Postgraduate Medicine. 2015. 127(3): 338-341.. Additionally there is a greater risk of exposing your partner to second-hand smoke, which can harm female fertility and the baby”s health during pregnancy. Vaping is also harmful for your health and the nicotine can reduce your sperm count 9 Oyeyipo IP, Raji Y, Emikpe BO, Bolarinwa AF. Effects of Nicotine on Sperm Characteristics and Fertility Profile in Adult Male Rats: A Possible Role of Cessation. Journal of Reproduction and Infertility. 2011. 12(3): 201-207..
Thankfully the damage done to sperm cells is reversible if you quit smoking altogether. This can be difficult to do, and you can get help from your GP as well as online resources.
Recreational drugs
Illicit substances can damage your health in various ways especially after long-term heavy use, and your sperm cells are not exempt from this.
Marijuana can reduce sperm production through the effects of tetrahydrocannabinol (THC), the drug”s psychoactive compound. Opioids can also harm fertility as they affect testosterone levels.
It is also important to remember that illicit drugs are rarely pure, and they are often mixed with other unknown harmful substances. Therefore to boost your sperm count, avoid taking illicit substances altogether.
Weight
Obesity can significantly reduce sperm count as it affects the hormone levels circulating in the body 10 Palmer NO, Bakos HW, Fullston T, Lane M. Impact of obesity on male fertility, sperm function and molecular composition. Spermatogenesis. 2012. 2(4): 253-263.. Another mechanism through which sperm count is affected is temperature, as obesity causes the testicular temperature to rise. This is particularly harmful for sperm cell development.
A high BMI is associated with reduced male fertility 11 Wang EY, Huang Y, Du QY, Yao GD, Sun YP. Body mass index effects sperm quality: a retrospective study in Northern China. Asian Journal of Andrology. 2017. 19(2): 234-237.. Therefore it is a good idea to exercise regularly and follow a healthy and balanced diet.
How to boost my sperm count
Unfortunately in many cases, the reason behind a low sperm count is unknown. Whether or not you know the cause of your low sperm count, the following actions can help you to improve your sperm count and your chances of conceiving:
– Quit smoking
– Cut down on how much alcohol you drink
– Avoid illicit drugs
– Exercise and maintain a healthy body weight
– Improve your diet to include a healthy intake of fruit and vegetables
– Avoid saunas and hot tubs
– Wear loose breathable underwear
– Make sure you get enough sleep and look after your mental health
– Avoid exposure to environmental toxins
– Have sex more frequently and synchronise this with your partner”s ovulation
– If you are using lubricants, use them sparingly as they can slow down sperm cells
– If you are taking medicines, ask your GP if they can affect your fertility
– Use a fertility supplement to boost your fertility
Conclusion
It is important to remember that having a low sperm count does not mean that you cannot have children. But it may take a little longer and require more effort from you to make sure you are as healthy as possible.
There are many changes you can make to improve your lifestyle and boost your chances of conceiving. But make sure you patiently wait to see the results of your hard work, because it can take around three months to see the improvement in your fertility.

Dr. Jones is an experienced consultant in assisted reproduction.
He has worked as a Fertility specialist at Kingston Hospital Assisted Conception and nearly 10 years experience of working in Obstetrics and Gynaecology across hospitals in the UK.
He completed his Masters in Assisted Reproduction Technology and then his PhD, from Imperial College London. Dr. Jones main areas of interest are Single Embryo Transfer, Endometriosis, PCOS and Implantation failure in IVF patients. He is a member of the British Fertility Society and an associate member of the Royal College of Obstetrics and Gynaecology.
Bibliography
- 1Levine H, Jørgensen N, Martino-Andrade A, Mendiola J, Weksler-Derri D, Mindlis I, Pinotti R, Swan SH. Temporal trends in sperm count: a systematic review and meta-regression analysis. Human Reproduction Update. 2017. 23(6): 646-659.
- 2Fawzy F, Hussein A, Eid MM, El Kashash AM, Salem HK. Cryptorchidism and Fertility. Clinical Medicine Insights: Reproductive Health. 2015. 9:39-43.
- 3Freeman HJ. Reproductive changes associated with celiac disease. World Journal of Gastroenterology. 2010. 16(46): 5810-5814.
- 4Wdowiak A, Bień A, Iwanowicz-Palus G, Makara-Studzińska M, Bojar I. Impact of emotional disorders on semen quality in men treated for infertility. Neuro Endocrinology Letters. 2017. 38(1): 50-58.
- 5Ilacqua A, Izzo G, Emerenziani GP, Baldari C, Aversa A. Lifestyle and fertility: the influence of stress and quality of life on male fertility. Reproductive Biology and Endocrinology. 2018. 16:115.
- 6Maleki BH, Tartibian B, Chehrazi M. The effects of three different exercise modalities on markers of male reproduction in healthy subjects: a randomized controlled trial. Reproduction. 2017. 153(2): 157-174.
- 7Gude D. Alcohol and fertility. Journal of Human Reproductive Sciences. 2012. 5(2): 226-228.
- 8Kovac JR, Khanna A, Lipshultz LI. The Effects of Cigarette Smoking on Male Fertility. Postgraduate Medicine. 2015. 127(3): 338-341.
- 9Oyeyipo IP, Raji Y, Emikpe BO, Bolarinwa AF. Effects of Nicotine on Sperm Characteristics and Fertility Profile in Adult Male Rats: A Possible Role of Cessation. Journal of Reproduction and Infertility. 2011. 12(3): 201-207.
- 10Palmer NO, Bakos HW, Fullston T, Lane M. Impact of obesity on male fertility, sperm function and molecular composition. Spermatogenesis. 2012. 2(4): 253-263.
- 11Wang EY, Huang Y, Du QY, Yao GD, Sun YP. Body mass index effects sperm quality: a retrospective study in Northern China. Asian Journal of Andrology. 2017. 19(2): 234-237.