For couples in the UK, poor sperm quality is the primary cause of approximately 20% of fertility problems. A further 25% of couples have trouble conceiving at least partially due to male sub-fertility. Evaluating semen and sperm quality is therefore the first and most obvious stage in trying to understand the cause of male sub-fertility.
The second stage is to look how to improve fertility. In many instances there is a range of medical options. However, focusing on good nutrition and certain nutrients can naturally improve fertility, plus enhance overall health and well-being.
What you will learn
What semen analysis is and how can it help you
The key readings count, morphology, motility, antibodies, volume, white blood cells and more
What you can do to improve your readings if they are diagnosed ‘suboptimal’
What is Semen Analysis?
The most effective way to determine the health of sperm is through a detailed analysis of a fresh semen sample. Results from semen analysis can help to identify specific fertility problems and steps that can be taken to improve fertility.
Although semen may be released in high volume, only 5% is made up of sperm. The remaining semen contains a range of fluids that are secreted throughout the genital tract. The highest percentage of sperm is concentrated within the first stage of ejaculation. This sperm is also the most mobile and more likely to fertilize the egg.
It”s important to understand that a semen analysis isn”t a complete fertility assessment. It”s not possible to assess all aspects of sperm function, such as the ability to find and fertilize an egg for example.
www.amitamin.com/en/fertilsan-m New life deserves the best possible start!We provide the essential building blocks for this.
Also, if the results indicate poor fertility, it doesn”t necessarily mean that natural conception isn”t possible. The ability to conceive will decline with increasing semen defects, although in most instances, there are steps that can be taken to improve semen health.
What actually happens?
Once the male has produced a sample, several aspects of the semen are investigated. The number of sperm (concentration), their shape (morphology) and movement (motility) are evaluated, as well as characteristics of the fluid, such as volume, white blood cell count and antibodies.
It”s important to mention that semen quality can be very variable between samples. For this reason, two or three samples are required to get an accurate analysis of semen quality and fertility. These samples should be provided several weeks apart.
Also, illness can impair semen count and function. It can take several months for semen quality to return to normal, especially after a high fever. In this case, specimens should be provided after a few months to ensure a more accurate result.
The figures below summarise the normal range for each of these parameters.
– Sperm concentration
More than 20 million sperm /ml
– Sperm morphology
More than 15% normal forms
– Sperm motility
More than 50% with forward movement
– Sperm antibodies
Less than 50% sperm with adherent particles
– Semen volume
More than 2.0 ml
– White blood cells
Less than 1 million cells /ml.
Understanding Semen Analysis Results
Sperm Concentration
Sperm concentration or count is determined by how many sperm are present within each millilitre of semen. A concentration in excess of 20 million sperm per millilitre is considered a healthy sperm count. Any figure below this is classified as a low sperm count (oligozoospermia).
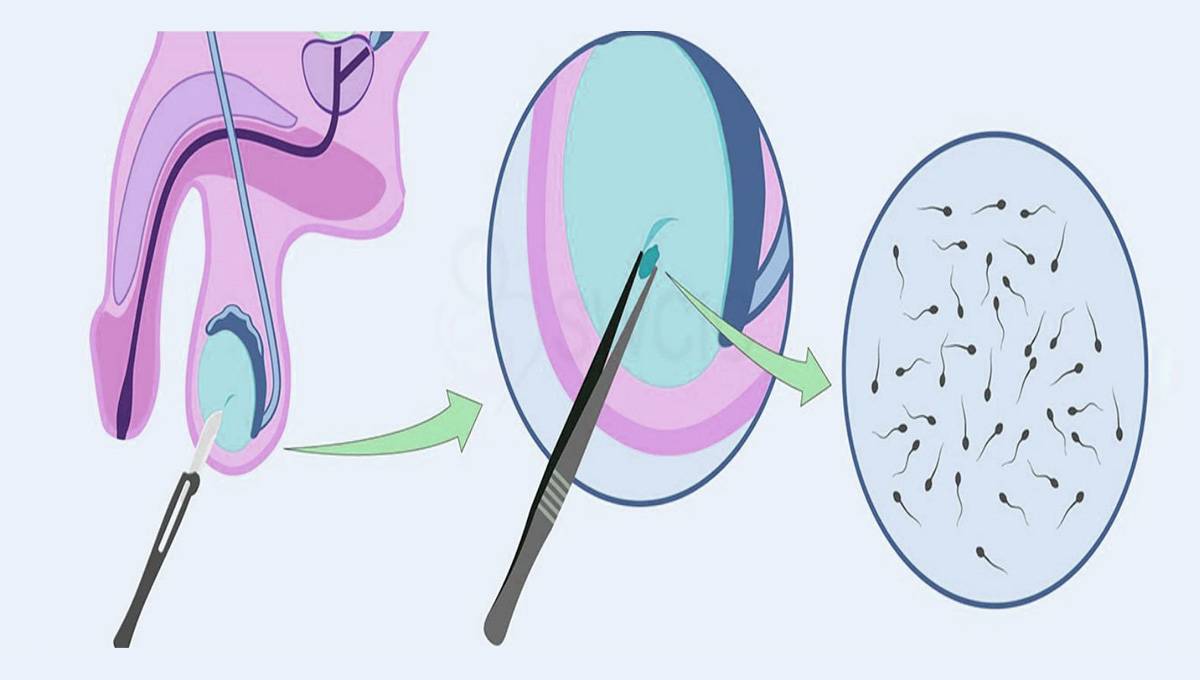
If no sperm is found in the analysis it”s possible that there is an obstruction preventing sperm flow or an absence of sperm production. Termed azoospermia, this medical condition affects approximately 2% of the male population.
Sperm Morphology
The ability to fertilize an egg is partly determined by sperm morphology. During semen analysis, sperm is expertly analysed under a microscope to assess tail, middle and head shape and proportions.
In humans, the ideal sperm shape, defined as “normal” sperm, is not produced in high concentrations, thus the lower limit of 15% normal sperm is considered acceptable. Once the percentage of normal sperm falls below 15% fertility also declines. Men with a normal sperm percentage of less than 5% will find conception especially difficult.
Find out 8 ways to boost SPERM MORPHOLOGY here
Sperm Motility
Although low sperm count is the most common reason for poor fertility, low sperm motility (asthenospermia) can also be a problem. Often these two characteristics occur together, making conception extra challenging.
A man is considered fertile by the World Health Organization (WHO) guidelines if he has a minimum “progressive motility”, i.e. grade a+b. of 32%, equivalent to 4.8 million/ml of semen (minimum WHO requirement sperm count of 15 million per ml x 32%). Vitality must be a minimum of 60% live spermatozoa1 Cooper TG, Noonan E, Von Eckardstein S, Auger J, Baker HWG, Behre HM, Haugen TB, Kruger T, Wang C, Mbizvo MT, Vogelsong KM. World Health Organization reference values for human semen characteristics. Human Reproduction Update. 2010. 16(3): 231-45.
Factors that can affect sperm motility include structural problems associated with the tail, sperm death (necrospermia) and autoimmunity against sperm.
Sperm Antibodies
This condition accounts for approximately 6% of male infertility. Sperm autoimmunity occurs when the body”s immune system attacks sperm as part of its natural defence mechanism against foreign organisms and substances.
Although sperm are normally protected from the immune system, some men produce antibodies that target sperm and reduce their lifespan. They attach to the surface of the sperm, reducing motility and the ability to penetrate the egg.
These antibodies can develop following some form of testicular trauma or surgery, such as a vasectomy. In many causes it isn”t possible to determine the trigger for the development of sperm antibodies. A simple immunobead test is done during semen analysis to detect concentration of antisperm antibodies.
Find out how to improve SPERM MOTILITY here
Semen volume
The volume of semen produced is measured to determine if there is a blockage of the seminal vesicles. Volumes less than 2 millilitres may indicate an obstruction preventing sufficient sperm concentration within semen and reducing fertility.
The most common cause of low semen volume is hormone imbalances. As men age, a decline in male sexual hormones will lead to the body producing less semen. Nutritional deficiencies, illness, injuries to the testicles, and infrequent sexual activity also reduce semen volume.

White Blood Cell Count
A high white blood cell count (greater than 1 million cells per millilitre) may be indicative of a genital tract infection which can damage sperm. Even though there may be no noticeable symptoms of an infection, a high white blood cell count will warrant further investigation and a possible course of antibiotics.
Other semen measurements
In addition to assessing white blood cell count, sperm vitality is also measured. A low percentage of living sperm can also suggest an infection or problems moving through the genital tract.
pH and fructose levels are also measured. Acidic semen (low pH) and/or the absence of fructose may suggest a blockage within the seminal vesicles and an alkaline semen (high pH) could indicate an infection. A pH between 7.2 and 7.8 is considered healthy.
Summary
Sub-fertility in men is very common and can be a source of anxiety. Undertaking a semen analysis will help to identify any problems with sperm production and sperm quality. Although semen screening can”t identify all potential causes for sub-fertility it will highlight the most common causes, such as a low sperm count, poor motility and morphology problems. By understanding the exact condition, it”s possible to take steps to improve fertility.
Take action now
Make several small behavioural changes such as minimising your swimmers’ exposure to heat, exercise more and eat more unprocessed foods,
Take a male fertility supplement. Several amino acids and trace elements, vitamins and vitaminoids have been proven very effective in improving sperm quality readings.
Male Fertility Supplements
Male fertility supplements are free of side effects, become effective after three to six months and are proven to increase sperm count by up to 215%, ejaculate volume by up to 33% and sperm motility by up to 23%2 Imhof M, Lackner J, Lipovac M, Chedraui P, Riedl C. Improvement of sperm quality after micronutrient supplementation. e-SPEN Journal. 2012. 7(1): e50-e53. Finally, they are relatively affordable. Whilst a varied diet is essential, supplements are able to deliver key nutrients in the required quantities more effectively and efficiently than any regular diet.
Supplements are therefore recommended for the initial treatment of asthenospermia (low motility) and oligospermia (low sperm count). A detailed yet easy to read paper summarising several studies was written by Steven Sinclair’s Male Infertility: Nutritional and Environmental Considerations.
Due to the lack of side effects to this form of natural “sperm boosting”, it is safe for men who have not been diagnosed with suboptimal semen analysis readings. They will benefit from supplementing micronutrients to ensure they can deliver high-quality semen.
The UK market has on offer a considerable range of male fertility supplements. However, the products differ widely in terms of nutrients and price.
Menfertility.org has carefully compared 24 of them in terms of value for money and the nutrient formula they provide.

Dr. Jones is an experienced consultant in assisted reproduction.
He has worked as a Fertility specialist at Kingston Hospital Assisted Conception and nearly 10 years experience of working in Obstetrics and Gynaecology across hospitals in the UK.
He completed his Masters in Assisted Reproduction Technology and then his PhD, from Imperial College London. Dr. Jones main areas of interest are Single Embryo Transfer, Endometriosis, PCOS and Implantation failure in IVF patients. He is a member of the British Fertility Society and an associate member of the Royal College of Obstetrics and Gynaecology.
Bibliography
- 1Cooper TG, Noonan E, Von Eckardstein S, Auger J, Baker HWG, Behre HM, Haugen TB, Kruger T, Wang C, Mbizvo MT, Vogelsong KM. World Health Organization reference values for human semen characteristics. Human Reproduction Update. 2010. 16(3): 231-45
- 2Imhof M, Lackner J, Lipovac M, Chedraui P, Riedl C. Improvement of sperm quality after micronutrient supplementation. e-SPEN Journal. 2012. 7(1): e50-e53